Accelerating Oncology Research: Unlocking the Power of AI and Real-World Imaging Data
Reading time /
4 min
Industry


Artificial intelligence (AI) is rapidly reshaping the arena of oncology research. AI can process massive amounts of complex data and generate relevant insights and improve workflows. In recent years, AI applications have extended well beyond genomic-based applications and now involve real-world imaging data (RWiD), which have the potential to redefine how tumors are detected, characterized, and monitored through treatment. Real-world imaging applications are more sophisticated than previous systems that were based on claims or electronic health records because they reveal the dynamic nature of tumor biology as it relates to spatial heterogeneity, changes post-treatment, and patterns of progression.
Recent advances in AI have led to the development of tools that have the capability to analyze millions of digital pathology slides and radiology images to recognize subtle features in tumors and novel biomarkers automatically. For instance, DeepHRD, an AI-enabled model has been demonstrated to identify homologous recombination deficiency in tumors from biopsy images with 1.8 to 3.1 times greater accuracy than genomic tests alone, and increase confidence in selecting targeted therapies. Additionally, beyond diagnostics, AI algorithms forecast responses to therapy, facilitate trial matching, and expedite timelines in drug development by identifying the correct subgroups of patients based on the phenotypes of their tumors.
The collaboration between AI and RWiD represents a critical moment in cancer research. It democratizes precision oncology's ability to personalize therapy to the individual patient through scalable, inclusive data that is generally outside the confines of clinical trials and specialized centers. By assessing tumor biology as it genuinely manifests, across patient outcome diversity and in real-world clinical practice, AI models are paving a new road toward the discovery of therapeutic vulnerabilities, monitoring treatment response, and ultimately enhancing outcomes across various cancers.
How AI is reshaping radiomics
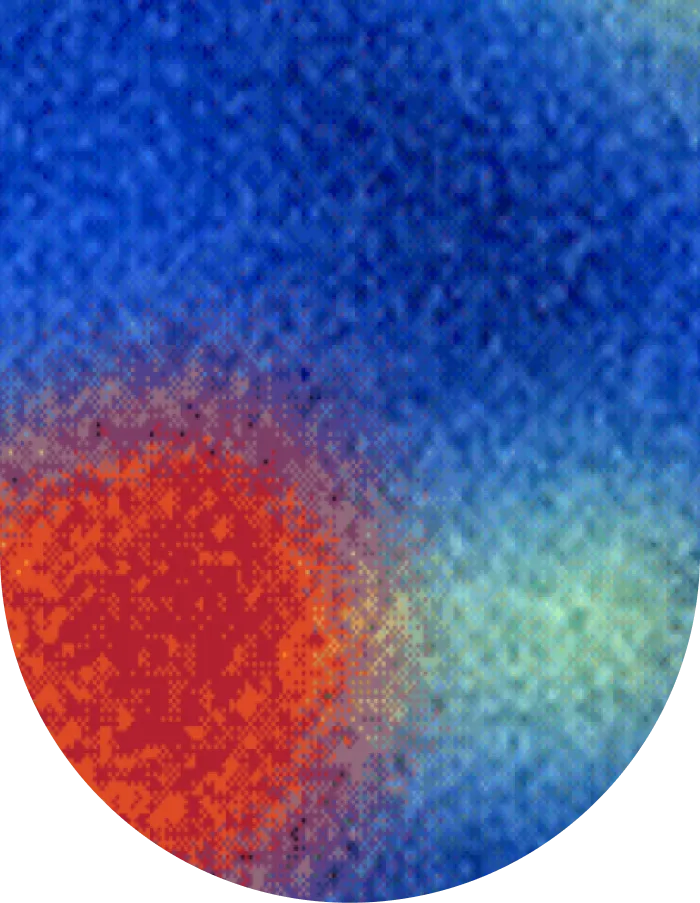
Radiomics has changed imaging in healthcare by developing quantitative features like intensity, shape, texture, and volume from routine radiology modalities. Radiomics began with hand-crafted features and made it possible to identify clinically relevant features that are not visually observable, and has been useful in tumor characterization, treatment planning and prognosis. Deep learning has built on radiomics by allowing models such as U-Net and ResNet to learn directly from the images. This opened the door to precise tumor detection, segmentation, and multimodal analysis to combine not only radiology, but also pathology and genomics. Today, AI is in standard clinical workflows with more than 700 FDA-approved radiology devices assisting with lesion detection, radiotherapy planning, and patient management.
The most recent advancement is with foundation models, large language models that are trained on large datasets and subsequently can be fine-tuned for specific tasks on smaller datasets. In the area of medical imaging, they are capable of accelerating research, increasing predictive power on limited cohorts of patients, and providing support for multimodal datasets that integrate image, report, and genomic data. Foundation models have established AI in a central position to enhance precision oncology through improved access, robustness, and clinical relevance of advanced analytics.
Considerations when building cancer AI research and clinical care tools
As AI is positioned to impact the future of cancer research and clinical care, we need to make sure any new tools are developed responsibly, safely, and effectively. Experts are clear that AI in oncology will depend on appropriate design, transparency, and collaboration as much as innovation. It is important to have a clear purpose when starting to develop an AI model. AI tools should always be developed to be useful, effective, and easy to use so that researchers or clinicians can integrate them into their existing workflow.
Recognizing limits is another important factor. It is important for developers to have an understanding of the situations in which the AI model works and does not work. Reviewing performance data is useful in avoiding overfitting and questionable outcomes of "too good to be true" results. Because transparency of outcomes engenders trust, it is important for researchers and clinicians who make decisions based on these models.
Ultimately, creating AI tools for cancer care involves more than strictly technical proficiency. There must be an intention for ethical innovation, transparency, and communal benefit. If these qualities of ethical innovation are upheld, the oncology field can apply AI for more efficient designs, better diagnostics, and to provide better and personalized care for patients with cancer.
Clinical applications of AI and RWiD in accelerating oncology research
Despite the recent technological advancement, cancer researchers are now looking into new opportunities for AI and RWiD, both opportunities to improve existing applications and opportunities to create new applications to expand the role of AI.
AI-enhanced imaging boosts both accuracy and speed of diagnosis
AI-enabled algorithms have been created to evaluate many different imaging modalities including MRIs, CT scans, mammograms, and PET scans, employing deep learning methods to identify small patterns that may indicate cancer. The goal of these diagnostic AI models is not to replace radiologists, but to act as a second reader, decreasing the priority of normal exams in the reading list, or potentially even fully exclude normal exams from the reading list. With these automated evaluations, human error is limited, and sensitivity or specificity is improved as those tumors are diagnosed earlier and staged better. The earlier cancer is diagnosed, the better treatment options and the better chance of survival, which is where radiologists would benefit from AI assessment.
Personalized treatment through integrative multi-modal data
When using AI to treat multi-modal data (imaging, genomics, proteomics, clinical histories), we can more closely capture the unique biology of the individuals’ tumors. Recognizing the mutations and biomarkers will allow us to personalize therapy based on a person's cancer profile (targeted drugs/immunotherapy). Personalizing therapy increases not only the effectiveness of treatment but also decreases negative effects by precisely informing therapy planning with richer data about both the patient and the tumor being treated.
Using AI to enhance drug discovery
AI accelerates early drug discovery through simulations of drug and biomolecular interactions and it can scan thousands to millions of potential candidate compounds rapidly via computational models. This decreases reliance on costly and labor-intensive lab experimental work. The more promising drug candidates can be identified rapidly for preclinical testing, faster than the overall development timeline of oncology drugs.
Real-time image analysis for adaptive treatment planning
AI capabilities allow for segmentation, tumor volume measurements, and the extraction of a variety of radiomics features from imaging studies to observe tumor responsiveness in real-time while being treated. AI can also enable adaptive treatment changes with real-time information (e.g., changing a radiotherapy dose due to the shrinkage of the tumor or lack thereof, to reduce normal tissue injury while also increasing treatment specificity). Radiomics is, similarly, influenced by the ability to achieve a better understanding of tumor heterogeneity, predicting outcomes, and changes to therapies and their dose.
Immunotherapy, which uses the immune system to fight cancer, is also an emerging area of transformative potential for applications of AI. Models developed with AI evaluate the tumor microenvironment (TME) and can be trained to learn the spatial distributions of immune cells to forecast the predicted patients' response to immune checkpoint inhibitors (therapeutics that blockade PD-1/PD-L1) and optimize patient stratification for immunotherapy. In addition, through AI techniques, we can incorporate radiographic imaging features with molecular and clinical data and improve our understanding of immune phenotypes and immune evasion that can lead to resistance. This not only facilitates the development of novel immunotherapy strategies but can shape how the field of radiology and pathology functions today, especially with advancing precision oncology as a continuum.
Segmed’s advantage in providing R&D with regulatory-grade image data
As real-world imaging data takes center stage in oncology R&D, Segmed can address many of the challenges mentioned and assist researchers, clinicians, and pharmaceutical companies in yielding next-generation data and insights for breast cancer.
Segmed offers fit-for-purpose, regulation-grade imaging datasets for complex medical research needs. These datasets can be used with a variety of patient cohorts, and high-quality screening and diagnostic mammography, breast MRI, and pathology reports. We have access to over 100 million de-identified, multimodal datasets. By integrating imaging with EHR, claims, and pathology data, researchers can gain a more complete understanding of patients and cancer subtypes. All tokenized, enabling them to understand the natural history of breast cancer spanning real populations.
Segmed enables links with data across institutional boundaries while facilitating meaningful patient privacy through the implementation of tokenization and a strict anonymization policy. This practice creates maximum value for research while respecting compliance.


