Transforming Breast Cancer Screening: How AI and Real-World Imaging Data Enable Earlier Detection
Reading time /
4 min
Industry


Historically, clinicians detected breast cancer through physical examinations or self-examination by patients who felt a lump or other breast abnormalities, with breast cancer diagnosed after their visual progression. By the early twentieth century, imaging technology started to focus more on breast cancer, starting with X-ray imaging and advancing through decades of imaging research into mammography, ultrasound, and MR imaging. Using medical imaging as a screening method, allowed identification of breast tumors before symptom onset. Although these developments improved survival, there were still significant challenges, such as false-positive and false-negative results, radiologist variability between imaging studies, and limitations for dense breast tissue.
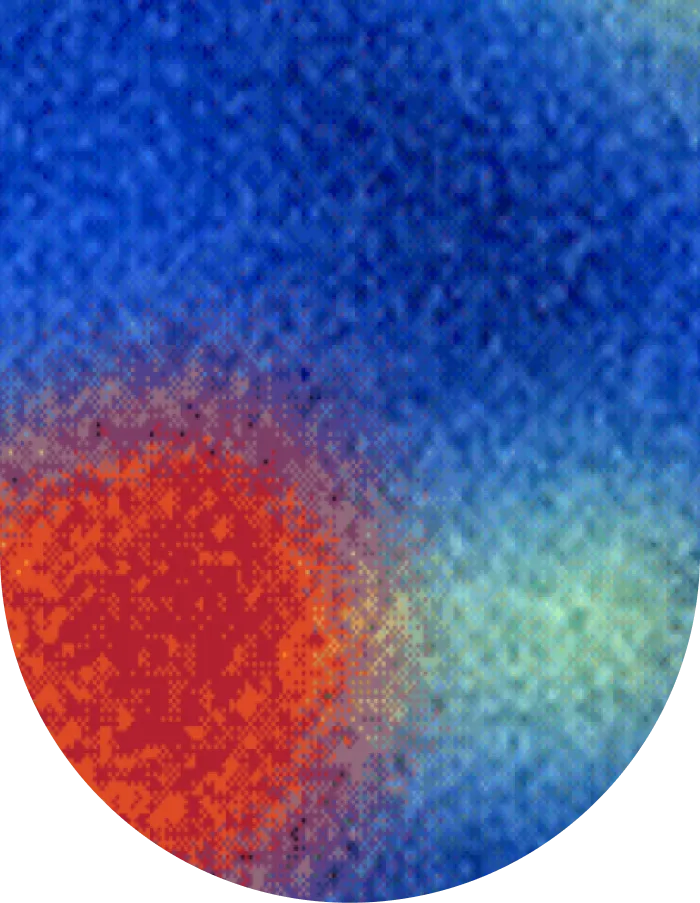
In the past few years, artificial intelligence (AI) and real-world imaging data (RWiD) have created a paradigm shift. AI models can currently evaluate mammograms and other breast images for subtle cancer-related changes, while real-world data ensures that these AI models are trained and validated based on scans reflective of true population diversity. This dual transformation allows breast cancer detection to change from a predominantly reactive, manual, and sometimes inequitable process to an increasingly proactive, automated, and equitable process.
Utilizing and enhancing AI for the identification of breast malignancies
For AI to have a substantive effect on the detection of breast cancer, several conditions must be satisfied. To begin, it must be integrated into the daily radiology workflow. The most appropriate algorithm should be applied, which is trained on real-world data from a representative population. Additionally, the AI model should continue to learn from new cases since characteristics may change over time (e.g. technology may change ,resulting in less noise or sharper images, which the AI model needs to be retrained on). When all of these conditions are satisfied, AI will work congruently with the clinical workflow, enabling radiologists to detect cancer earlier and lead to improved survival of patients.
Integrating AI into the workflow and its clinical effects
AI tools are meant to support, rather than replace, the work of radiologists. Breast cancer screening programs require either a single reader (e.g. USA) or two readers (e.g. Europe and Australia). In the realm of breast imaging, AI automates the detection of lesions, can triage cases by risk, and can quickly generate quantitative metrics such as the size and shape of the tumor. Implementations of AI into multisite mammography screening have shown that AI can increase cancer detection rates, decrease false positives, and lessen the radiologist workload. Collaborative “AI-plus-radiologist” models leverage triage, support decision-making, improve screening metrics, and potentially reduce fatigue. AI may enable two reader breast cancer screening programs to transition to a single reader program.
Detection driven by advanced algorithms
Conventional computer-aided detection methods resulted in limited accuracy. Deep learning frameworks such as convolutional neural networks (CNNs) have improved accuracy substantially and are therefore now at the heart of the AI-based applications for breast imaging. CNNs efficiently extract sophisticated image features in order to distinguish benign from malignant lesions.
Data and annotating Real-World Medical Imaging
Strong model performance relies on a wide variety of large and diverse datasets. Large uniform collections of mammogram images, which have been clinically verified from multiple institutions and patient populations, can act as reliable training and validation data. Those images will also have diversity in imaging devices, patient population, and imaging protocols, which can help promote generalizability and reduce bias in models. Standardizing annotation by staff or medically approved tools, especially with detailed annotation, will allow AI to better learn more subtle imaging patterns related to the detection of early-stage cancers.
Validation, performance metrics, and continuing education
Important performance metrics, such as sensitivity, specificity, area under the curve (AUC), and false positives/negatives, are key to assessing the performance of AI models. Prospective studies have shown that AI-assisted reading of imaging data (e.g. AI-derived blueprints read by radiologists) can improve detection rates, although recall rates remain unchanged. Continuous training of AI systems (retraining the system on new real-world imaging data) helps AI systems to meaningfully improve and adapt to new and changing technology and populations, and sustain accuracy over time.
The practical application of AI in breast cancer screening: getting answers for patients and researchers faster
Although many AI systems have been developed within a research paradigm, advances in care need to be demonstrated when they are implemented, mostly in routine clinical practice. Here are exemplary examples of how AI and real-world imaging data are changing the breast cancer screening landscape related to detection, risk stratification, and equity of care.
Nationwide multicenter implementation
A large retrospective real-world data study evaluated AI as an independent reader in double reading across 275,900 mammograms from multiple screening centers and imaging vendors. The analysis showed that AI was non-inferior to standard human double reading for cancer detection and recall rates, while demonstrating consistency across different equipment types and clinical settings. These findings support the potential of AI to safely integrate into existing breast cancer screening workflows and to scale across diverse healthcare environments.
Advanced AI risk models
Recent artificial intelligence-driven risk models have shown the ability to improve breast cancer risk prediction compared with traditional clinical models. By analyzing current and prior mammograms, along with established risk factors such as age and breast density, these models can more accurately predict future breast cancer risk than standard approaches like the Breast Cancer Surveillance Consortium (BCSC) model. Large retrospective studies across health systems, including cohorts of more than 300,000 women, demonstrated improved discrimination for both short-term and 5-year risk, and newer models that incorporate longitudinal mammographic history further enhance prediction performance. While prospective trials of risk-based screening strategies are still in early stages, simulation studies suggest that such approaches could enable more personalized screening intervals and reduce both under-detection and unnecessary imaging.
AI validation success
Multiple software as a medical device (SaMD) companies have validated their AI models using Segmed’s database. Applying Segmed’s technology on the diverse and heterogeneous network of healthcare providers allowed for building high quality fit-for-purpose datasets used by our clients to validate their models. This allowed assessment of generalizability of AI models.
Segmed’s advantage in providing R&D with regulatory-grade image data
As real-world imaging data takes center stage in oncology R&D, Segmed can address many of the challenges mentioned and assist researchers, clinicians, and pharmaceutical companies in yielding next-generation data and insights for breast cancer.
Segmed offers fit-for-purpose, regulation-grade imaging datasets for complex medical research needs. These datasets can be used with a variety of patient cohorts, and high-quality screening and diagnostic mammography, breast MRI, and pathology reports. We have access to over 100 million de-identified, multimodal datasets. By integrating imaging with EHR, claims, and pathology data, researchers can gain a more complete understanding of patients and cancer subtypes. All tokenized, enabling them to understand the natural history of breast cancer spanning real populations.
Segmed enables links with data across institutional boundaries while facilitating meaningful patient privacy through the implementation of tokenization and a strict anonymization policy. This practice creates maximum value for research while respecting compliance.


